Prostate Cancer
Prostate
The prostate is a walnut-sized gland that makes prostatic fluid and stores seminal fluid. It is located between the bladder and the penis, and encircles the upper part of the urethra (the tube that empties urine from the bladder) like a donut. The prostate helps regulate bladder control and sexual function.
What is prostate cancer?
Prostate cancer is a malignant (cancerous) disease that affects the cells of the prostate. 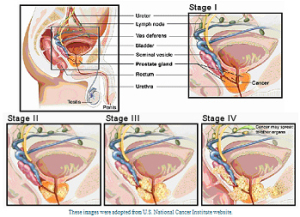 A malignant growth has the potential of spreading to other tissues of the body and can cause damage to surrounding tissue or break away and spread to other parts, such as the lymph nodes. Prostate cancer is the second-leading cause of cancer deaths (after lung cancer) among men in the United States. It is more common in African American men and in men with family history of the disease. Causes of the disease are unknown. The mortality rate has declined more than 25 percent in recent years due to early detection and modern techniques that have also contributed to an improved quality of life. In its early stages, prostate cancer may not cause any symptoms, however as it progresses several symptoms may appear, such as frequent urination (especially at night), problems with urination, painful ejaculation, blood in the urine or semen, back and hip pain and stiffness.
A malignant growth has the potential of spreading to other tissues of the body and can cause damage to surrounding tissue or break away and spread to other parts, such as the lymph nodes. Prostate cancer is the second-leading cause of cancer deaths (after lung cancer) among men in the United States. It is more common in African American men and in men with family history of the disease. Causes of the disease are unknown. The mortality rate has declined more than 25 percent in recent years due to early detection and modern techniques that have also contributed to an improved quality of life. In its early stages, prostate cancer may not cause any symptoms, however as it progresses several symptoms may appear, such as frequent urination (especially at night), problems with urination, painful ejaculation, blood in the urine or semen, back and hip pain and stiffness.
How is prostate cancer diagnosed?
The goal of prostate cancer screening is to evaluate and diagnose the disease in its early stages. Physicians routinely use two types of exams to screen men for prostate cancer. The first type is a called a digital rectal exam (DRE), in which a doctor inserts a gloved finger into the rectum to feel the prostate for irregularities. The second, a blood test, detects the amount of prostate-specific antigen (PSA) in the blood. Men with non- cancerous benign hyperplasia (BPH) may also have elevated PSA levels. A prostate biopsy is performed in our office if the PSA levels, either remain elevated or continue to rise. The tissue from the biopsy are sent to a pathologist who will grade the cancer using a measuring method called the Gleason grading, named after its founder Dr. Gleason. This grading system helps us determine the type of therapy that is best for you. Grade 1 is the least aggressive and looks a lot like normal prostate tissue, but has distinguishing features identifiable as cancer. Grade 5, however is the most aggressive and does not resemble normal tissue. Along with grading the cancer, we use a staging method to determine how advanced the cancer is at the current time. Common tests used to identify this might include a bone scan or a CT scan of the pelvis.
a gloved finger into the rectum to feel the prostate for irregularities. The second, a blood test, detects the amount of prostate-specific antigen (PSA) in the blood. Men with non- cancerous benign hyperplasia (BPH) may also have elevated PSA levels. A prostate biopsy is performed in our office if the PSA levels, either remain elevated or continue to rise. The tissue from the biopsy are sent to a pathologist who will grade the cancer using a measuring method called the Gleason grading, named after its founder Dr. Gleason. This grading system helps us determine the type of therapy that is best for you. Grade 1 is the least aggressive and looks a lot like normal prostate tissue, but has distinguishing features identifiable as cancer. Grade 5, however is the most aggressive and does not resemble normal tissue. Along with grading the cancer, we use a staging method to determine how advanced the cancer is at the current time. Common tests used to identify this might include a bone scan or a CT scan of the pelvis.
Prognosis translates into your chances of cure/long-time survival and is largely based on your grade, stage and PSA. Most patients are very curable; it is only a minority of patients who present with the disease that is already incurable.
What are my treatment options?
Various treatment options are available for prostate cancer, each with its own benefits especially for high-grade cancers, while observation called watchful waiting may be more appropriate for low-grade cancers, elderly patients or patients with other medical conditions. Surgical procedures called prostatectomy, which involves the removal of the entire prostate gland, is the most common form of treatment with the intent to cure prostate cancer. Radiation therapy, hormonal therapy, and cryosurgery or freezing the prostate are other forms of treatment. As your physician, it is my responsibility to inform you of the various treatment options that are available based on your individual evaluation.
Radical Prostatectomy:
A radical prostatectomy means removal of the entire prostate and seminal vesicles. Because prostate cancer is scattered throughout the prostate gland in an unpredictable way, removal of only part of the prostate would leave cancer cells behind. The pelvic lymph nodes that filter the lymphatic fluid from the prostate are usually the first site of any spread of the cancer beyond the prostate gland. These lymph nodes are also removed during this operation. Fortunately, you have many other lymph nodes, so your body will not miss these few. The primary purpose of the operation is to cure the cancer by removing it completely, while making every effort to preserve normal functions. I will recommend several prostatectomy procedures depending on our findings.
Robotic Surgery:
 One of the newest minimally invasive surgical techniques includes using a robot called the daVinci Surgical System. This procedure is performed by making five small incisions (ports) into the abdomen and inserting surgical instruments through ports to carry out the procedure. I actually control the robot from the computer terminal in the same room as the patient but not at the patient site. I have an assistant who stands at the side of the patient, bringing in new instruments and helping with visualization, should there be small amounts of bleeding in the surgical field. Results from this surgical procedure are excellent. In the hands of an experienced robotic surgeon, they should be equivalent to the open technique. In my hands, cancer control is the same as the more traditional open technique and quality of life outcomes are equal or perhaps slightly better. Patients return to normal function and activity in a shorter period of time. This is due to significantly less blood loss and small incisions that lead for a quicker recovery. Patients are able to resume most normal activities within 2 weeks after the operation, and all normal activities 3 weeks after the operation, unless, of course, they have had some major postoperative complication that lengthens the period of recovery. Hospitalization is generally 1-2 nights after the operation. The patient is discharged home with a catheter in the bladder, after they are successfully passing flatus.
One of the newest minimally invasive surgical techniques includes using a robot called the daVinci Surgical System. This procedure is performed by making five small incisions (ports) into the abdomen and inserting surgical instruments through ports to carry out the procedure. I actually control the robot from the computer terminal in the same room as the patient but not at the patient site. I have an assistant who stands at the side of the patient, bringing in new instruments and helping with visualization, should there be small amounts of bleeding in the surgical field. Results from this surgical procedure are excellent. In the hands of an experienced robotic surgeon, they should be equivalent to the open technique. In my hands, cancer control is the same as the more traditional open technique and quality of life outcomes are equal or perhaps slightly better. Patients return to normal function and activity in a shorter period of time. This is due to significantly less blood loss and small incisions that lead for a quicker recovery. Patients are able to resume most normal activities within 2 weeks after the operation, and all normal activities 3 weeks after the operation, unless, of course, they have had some major postoperative complication that lengthens the period of recovery. Hospitalization is generally 1-2 nights after the operation. The patient is discharged home with a catheter in the bladder, after they are successfully passing flatus.
HIFU Treatment
A recently approved therapy called HIFU (high intensity focused ultrasound) is now available. This has been used in Europe for 20 years and is now available here. It is very effective and I prefer it to cryosurgery. High Intensity Focused Ultrasound (HIFU) is a minimally-invasive ablation therapy which can be used to treat localized prostate cancer. Learn more about HIFU Treatment here.
Why do complications happen? What do you mean by risk management?
Watching the evening news, we hear about unfortunate events on a steady basis: floods, tornadoes, stock market crashes, terror attacks and street crime, motor vehicle accidents, plane crashes and oils spills. The world is an unpredictable place and even those who do not expect or deserve suffering are at times subjected to it. As long as we live, we are surrounded by risks. Some risks are perceived to be greater than what they really are; some are present and real. We do not like to hear about these untimely events because they challenge our perceived feelings of being in control at all times.
We are more afraid of situations that we cannot control like flying, having surgery, than of situations we can control, such as driving a car, smoking, overeating even though the latter may carry a significantly higher risk. Statistically, it is safer to fly than it is to drive a car! Many people are more afraid of dying from cancer than from cardiovascular disease even though twice as many people die from cardiovascular disease! Therefore, before any important decisions are made, a careful risk assessment must be done and benefits must be put in perspective. Strategies should be sought to maximize benefits and minimize risks.
Medicine has come a long way. Historically, humans have never lived as long as they do today. New research and medical technology hold great promises for the future. Nevertheless, the human body is a complex biological system. We have a good understanding of cause and effect, and depending upon the question or problem at hand, physicians are correct many or even most of times in predicting medical outcomes.
Unfortunately, even in expert hands, some outcomes or complications are an unavoidable consequence of surgical practice involving not only one but several complex biological and technical systems (people) and platforms (technical equipment). Even when the surgery is in the most experienced hands, factors related to the patient like anatomical variations, extent of preexisting, or unrecognized disease, factors related to the operating room environment, or equipment forces can lead to a postoperative complication. Nonetheless, I have done thousands of prostatectomies. I am dedicated to the pursuit of a perfect outcome in all my patients, although, a complication or adverse event may occur. Therefore, to minimize the chance of complications, I recommend choosing an expert surgical and medical team that performs surgical procedures on a very frequent basis, in a high quality setting, and one that has all the equipment and brainpower at the hand should there be a complication.
As your surgeon, consultant, and advocate, my pledge to you is that we take your safety personally, will discuss with you risks and benefits of this procedure, and will carefully preplan your case, execute your surgery in a highest quality fashion. I will monitor you closely for potential postoperative problems. While the overwhelming majority of what we do goes as expected, I will be available to guide you through any potential complications, explain problems, and based on my experience formulate a plan to deal with what is at hand. Even if complications occur, the consequences can often be minimized through early recognition and appropriate intervention.
What to expect after surgery
Urinary Control:
Patients are normally discharged from the hospital with a catheter in place. The catheter is left in place for approximately one week after surgery. This gives the Anastomosis, or union between the bladder and urethra, time to heal completely. I perform an x-ray called a cystogram prior to removal of the catheter. The catheter is removed in our office and you will be given instructions on exercises called Kegel to begin at home. Urinary control is of paramount importance prior to surgery. Bio-feedback training is highly recommended.
Recovery and return of urinary control is an area that is difficult to predict for each individual patient. In my patient population, I have found that the average man are dry or nearly completely dry 2 to 8 weeks after the Foley catheter has been removed. Nearly completely dry means they are wearing one pad or less per day. Other men take as long as 3 to 6 months to get dry, and there is certainly a small group of men, who, as I will discuss, do not get completely dry for various reasons. There are ways to manage this usually mild leakage of urine (that is nonetheless very troubling). Different methodologies are incorporated to try and return men to their complete urinary control as quickly as possible, but it is impossible to predict for each individual patient what their recovery time may be.
On my team are specialist in correcting urinary incontinence, Dr. Rose Khavari and Dr. Julie Stewart.
I look forward to discussing this in greater detail with you during your consultation.
Study Information
Preoperative Biofeedback Assisted Behavioral Training to Decrease Post-Prostatectomy Incontinence: A Randomized, Controlled Trial
Kathryn L. Burgio and corresponding Author Information email address, Patricia S. Goode and, Donald A. Urban MD, Mary G. Umlauf, Julie L. Locher MD, Anton Bueschen, David T. Redden
Purpose
We tested the effectiveness of preoperative biofeedback assisted behavioral training for decreasing the duration and severity of incontinence, and improving quality of life in the 6 months following radical prostatectomy.
Materials and Methods
We performed a prospective, randomized, controlled trial comparing preoperative behavioral training to usual care. The volunteer sample included 125 men 53 to 68 years old who elected radical prostatectomy for prostate cancer. Patients were stratified according to age and tumor differentiation, and randomized to 1 preoperative session of biofeedback assisted behavioral training plus daily home exercise or a usual care control condition, consisting of simple postoperative instructions to interrupt the urinary stream. The main outcome measurements were duration of incontinence (time to continence), as derived from bladder diaries, incontinence severity (the proportion with severe/continual leakage), pad use, Incontinence Impact Questionnaire, psychological distress (Hopkins Symptom Checklist) and health related quality of life (Medical Outcomes Study Short Form Health Survey).
Results
Preoperative behavioral training significantly decreased time to continence (p = 0.03) and the proportion of patients with severe/continual leakage at the 6-month end point (5.9% vs 19.6%, p = 0.04). There were also significant differences between the groups for self-reported urine loss with coughing (22.0% vs 51.1%, p = 0.003), sneezing (26.0% vs 48.9%, p = 0.02) and getting up from lying down (14.0% vs 31.9%, p = 0.04). No differences were found on return to work and usual activities or quality of life measures.
Conclusions
Preoperative behavioral training can hasten the recovery of urine control and decrease the severity of incontinence following radical prostatectomy.
Sexual Preservation:
Every attempt is made to keep men as sexually capable coming out of the operation as they are going in. Sexual preservation, of necessity, requires a number of different therapies that will be used to keep you sexually active and normally potent. These efforts, led by my colleague Dr. Mohit Khera involve starting oral drugs called 5-phosphodiesterase inhibitors. These are the drugs commonly known as Viagra, Cialis, or Levitra, and are given to help maintain and preserve sexual function and to improve healing along the neurovascular bundles, which often get bruised to some degree. I also encourage the use of vacuum erection devices to stimulate and exercise the penis, and other pharmacologic measures, such as the instillation of small amounts of the drug called prostaglandin E1 in the form of a suppository placed just inside the opening of the penis. Another tool is the direct introduction of medications called Tri-mix by a very small #32-gauge needle (somewhat bigger than a hair).
It is important to me that you return to sexual activity in as short a period as possible after the operation. To that end, if you are not sexually active within 2 to 3 months after the operation, I will have you seen by one of my associates.These individuals specialize in male potency and are some of the leading investigators in new methodologies for helping the male with erectile problems return to normal function. I am a complete believer in the team concept. I am a cancer specialist and strongly believe that the best minds in each discipline should be brought to bear on your health and in returning you to a normal life. Therefore, one of these gentlemen may be involved in your care in order to help in the preservation of your sexual activity.
Nerve Sparing
As a patient, you may read about two forms of nerve-sparing procedures. One is referred to as intrafascial and other as extrafascial. Extrafascial is the more standard nerve-preservation technique. The prostate lives under a plane of tissue called the endopelvic fascia. Fascia are thick layers of tissue that separate various organs from other structures. It also separates the body into different compartments (all muscles are confined within fascial layers). We normally will open the endopelvic fascia in order to better expose the sides of the prostate. This dissection involves getting into the fascial plane toward the side of the prostate, or laterally. The rest of the dissection then moves medially toward the prostate into a fascial plane between the prostate and the neurovascular bundles.
The intrafascial technique is used for much lower volume disease in a very select number of patients. During an intrafascial dissection the endopelvic fascia is never opened laterally. We simply approach the neurovascular bundles from the prostate side sweeping up under the prostate between the neurovascular bundle and the prostate so that we never touch the lateral aspect of the neurovascular bundle. There is a belief that this therefore causes less traction and less injury to the neurovascular bundle since we are only approaching it from one side and not both sides. My personal belief in reviewing my patients is that it does help in obtaining a quicker return of potency for the average patient. Of course, every person is individual and there is no way to predict in whom this will be helpful. I do believe that it also helps return of urinary control to be achieved much more quickly.
Biochemical Recurrence
Although we are able to cure most prostate cancers and in some of the earlier stages with less aggressive tumor, veritably all patients, nonetheless, some patients will recur. The percentage of patients who recur will vary substantially based on final pathologic stage after the prostate is removed. Final pathologic stage means when the pathologist looks at the tissue and tell me how extensive it is, whether it involves certain parts of the specimen such as the seminal vesicles and/or lymph glands. All of those have a direct bearing on the possibility of recurrence of disease. As I may have mentioned earlier, the way that we are able to follow prostate cancer after treatment, especially by removal of the prostate, is by following the PSA. After prostatectomy, the prostatic-specific antigen should go to undetectable levels. Undetectable means less than 0.1 ng/ml. Many patients will ask me, “Well, how can I have a PSA at all, since I don’t have a prostate?” The explanation is the PSA is not made by the prostate but by prostate cells. Each prostate cell makes a little bit of PSA. As the number of cells increases, the level of PSA will rise. The more cells, the more PSA. If prostate cancer cells remain in the area around the prostate, known as the prostatic bed, or inthe lumphatic channels, they will produce enough PSA that we can measure it. That is, the PSA now becomes detectable. This is called a biochemical recurrence. The number of cell is dramatically small relative to our ability to detect it beyond the blood test. At this point there is not enough cancer to be seen by any form of x-ray. Nonetheless, we know that it is present. By and large, this is usually a local recurrence and after surgery patients are given radiation therapy to the prostatic bed and periprostatic lymphatic channels. This is very frequently successful. The side effects from what is called salvage radiation therapy are generally quite mild. We will talk about this in great detail during our visits and with the radiation oncologist, should that become necessary.
Retzius-Sparing Procedure
Recently another technique has been developed for the performance of a robotic-assisted prostatectomy. Normally, we drop the bladder from the anterior abdominal wall into the abdominal cavity and then approach the prostate from above the bladder. That would be behind and under the bladder, which I will discuss with you at the time of the consultation. The theory of this technique is that less manipulation and mobilization of the bladder and pelvic structures will help with urinary control. The thought is the normal anatomy is less apt to be injured or violated if we leave everything in place and simply remove the prostate from underneath and behind the bladder. The data on this is growing, but the number of people able to perform the procedure is quite small at this time. For selective patients this may be a reasonable option.
Nomograms
A nomogram is simply a tool to aid a patient or doctor in predicting various outcomes before or after treatment.
Memorial Sloan Kettering Cancer Center’s free prostate cancer prediction tool. Will open a new page.
The first nomogram developed for prostate cancer — called the Kattan-Partin nomogram — was developed to predict final pathologic stage; that is,
Memorial Sloan Kettering Cancer Center’s free prostate cancer prediction tool. Will open a new page.
whether or not a cancer will be confined completely within the prostate or extend beyond the limits of the gland. Despite being somewhat useful, this tool is far from perfect. The reason for this is that there is a fair amount of “lumping” done. That is the groups categorized are quite large. For instance, if your PSA is between 6 and 10, your Gleason score 3+3,
and your stage T1c (found due to an elevated PSA), your chance of having organ-confined disease is 75 percent, but this “lumps” all patients with these parameters, whether you have one small focus in one biopsy core positive for cancer or whether all 12 cores are positive for cancer.
I therefore encourage you to be careful in looking at these numbers and drawing profound conclusions from them. In addition, please recognize that in this particular nomogram, a 30% chance of having cancer outside the prostate does not equate with only a 70% chance of cure. For relative ideas of cure, please use the Kattan pre- and postoperative nomograms. There are many other nomograms that are developed, which incorporate various biologic or pathologic or laboratory testing that are unique for radiation and/or surgery and predicting the outcomes from these. The number escalates geometrically each year, and the usefulness of each of these in truly predicting future outcomes for any patient is not known and therefore should be used guardedly and with caution.
I made a number of these nomograms accessible, and please feel free to put in your particular parameters. More importantly, however, I look forward to discussing with you during your office visit the significance of each of these and what you might anticipate in your own particular situation.
Contact Info
Scurlock Tower Suite 2100
6560 Fannin Street
Houston, Texas 77030
Phone: (713) 441-6455
Fax: (713) 790-4456
info@drbrianmiles.com
Map and Directions

